The term ‘treatment' refers to any medical, surgical or dental treatment or other health care, including a life-sustaining measure or palliative care.
In the Act, for the purpose of Part 9B (Advance health directives) and Part 9E (Medical research), the term ‘treatment’ includes medical research. Medical research is not included in the definition of treatment when it is applied to other parts of the Act.
For more information refer to the Position Statement: Decisions about medical research.
Responsibility for ensuring capacity
Responsibility for ensuring that a person understands the nature and consequences of the treatment proposed - and for obtaining a treatment decision - lies with the health professional.
If a health professional has concerns about the capacity of a person who has not made an AHD and for whom nobody in the hierarchy of treatment decision-makers can be found below, they might need to consider applying to the State Administrative Tribunal for the appointment of a guardian.
Urgent treatment
Show moreTreatment is regarded as urgent if it is needed to save a person's life or prevent the person from suffering significant pain or distress.
Where a person requires urgent treatment and it is not practicable for the health professional to determine whether an Advance Health Directive (AHD) has been made or to obtain a treatment decision from anybody in the hierarchy, the health professional may provide the necessary treatment.
Urgent treatment - following attempted suicide
When a person is in need of urgent treatment, that the health professional believes is the result of attempted suicide, they may administer the necessary treatment even:
- if the person has made an Advance Health Directive in which consent for the required treatment is withheld
- the person's guardian, enduring guardian or person with authority to make a decision withholds consent.
Non-urgent treatment and Advance Health Directives
Show moreIf you have an Advance Health Directive
If a person in need of non-urgent treatment has made an AHD and the directive covers the treatment required, the health professional will need to proceed in accordance with the directive. There are some circumstances where the AHD may be considered invalid, in which case the health professional may not follow the directive.
Validity of Advance Health Directive
If circumstances have changed since making an AHD, this can affect its validity. For example, a treatment that wasn’t available at the time of drafting, may now be a valid option, but it wasn’t factored into the AHD. In such cases the AHD could be judged invalid
A range of factors would be considered when determining the validity of the AHD including:
- the person's age at the time they made the AHD
- whether the person had reviewed their AHD since it was made and, if so, how long it had been since the review was undertaken
- the nature of the condition for which the person required treatment, the nature of the treatment itself and the consequences of providing (or not providing) that treatment.
For more information on Advance Health Directives and their validity, go to the Department of Health's website.
If you do not have an Advance Health Directive, or it is invalid
If a person has not made an AHD (or if it is invalid), the legislation sets out the order of people who the health professional will need to obtain a treatment decision from. This order is contained in sections 110ZJ and 110ZD of the Act and has been summarised for ease of understanding as 'the hierarchy of treatment decision-makers'.
The hierarchy of treatment decision-makers
Show more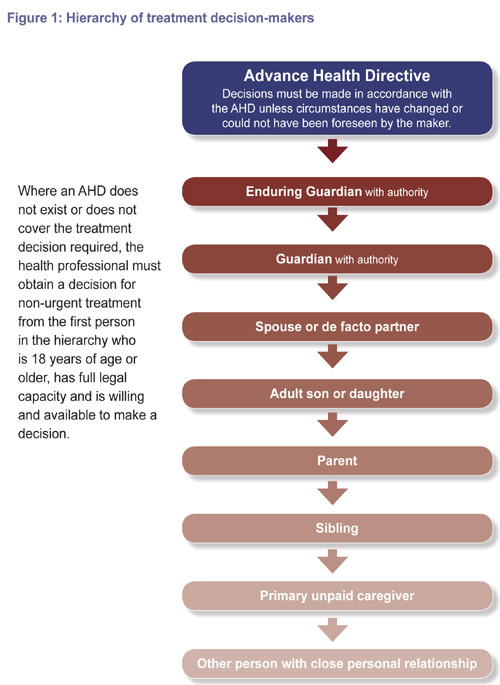
When obtaining a treatment decision, the health professional must go to the first person on the hierarchy, who is:
- 18 years of age or older
- has full legal capacity
- is reasonably available
- willing to make the decision.
If all of these conditions are not met, for example the first person in the hierarchy does not have capacity or is not available, the health professional can go to the next person in the hierarchy.
A health professional must consult the nearest relative in the order above, before moving onto a primary unpaid carer.
It does not matter whether the spouses or de facto partners are different sexes or the same sex; or if either of the persons is legally married to someone else or in another de facto relationship. The Acts Amendment (Lesbian and Gay Law Reform) Act 2002.
There is no distinction in relation to age, therefore all children of a person have equal priority, and a health professional does not have to seek a treatment decision from the eldest child.
A person is to be regarded as maintaining a ‘close personal relationship’ with the person needing treatment if the relationship is maintained through frequent personal contact and a personal interest in the welfare of the person needing the treatment.
When to apply for a guardianship order
Show moreThere are a number of treatment-related circumstances where, in the view of the Public Advocate, an application for a guardianship order should be made to the State Administrative Tribunal including:
- where treatment is required and there is no AHD and no person who comes within the description of S110ZJ and 110ZD of the Guardianship and Administration Act 1990
- the person authorised to make a treatment decision is unwilling to make a decision or cannot be contacted
- there is conflict about the adult's capacity to make a treatment decision for the proposed treatment
- the person for whom the treatment is proposed objects to the treatment.
An application must be made to the State Administrative Tribunal when an adult lacks the capacity to make a treatment decision regarding a sterilisation procedure.
Treatment Decisions – the role of the Public Advocate
Show moreWhen no one else is willing, suitable and available to act as guardian, the Public Advocate may be appointed by the State Administrative Tribunal as guardian of last resort with authority for treatment and health care.
The Public Advocate as guardian must:
- Advise health professionals of their responsibilities to seek treatment decisions from the Public Advocate.
- Advise all allied health staff and carers, who provide treatment or administer medication, of the Public Advocate's treatment and health care authority.
- Gather all relevant information to help make decisions about the person's treatment or health care and the cost of such treatment or care. This includes the expressed views of the person or such views as can be gained by their previous actions. This information may be gathered from the person affected, from family members, the treating health professional, carers, service providers, the administrator or attorney of the person affected and other interested parties.
- Obtain a copy of a valid Advance Health Directive, where available.
- Make decisions about the person's treatment or health care.
The Public Advocate may also:
- request and/or attend case conferences and review meetings to discuss health care matters
- attend a medical appointment between the represented person and their treating doctor to gain more information about complex treatment decisions and the views of both parties
- request written reports following medical (or other health) reviews and assessments
- consider a second medical opinion as part of the process for determining what treatment decision to make.
- request a treatment plan, when the represented person is admitted to a health care facility or when major health concerns have been raised or diagnosed
- where necessary, make complaints to appropriate authorities, on the person's behalf, about health care matters
- seek directions from the State Administrative Tribunal regarding a person's treatment and health care, where appropriate
- apply to the State Administrative Tribunal for medical research authority if there is no one else suitable, available or willing to make a medical research decision under Sections 110ZP and 110ZQ of the Act.
The Public Advocate does not take the place of relatives, friends, carers or paid service providers in helping the person with a decision-making disability. It is important that the person continues to receive the services, support and care provided by service providers, family and friends.
The Public Advocate does not:
- make treatment decisions without information from the treating health professional
- make practical arrangements for medical appointments, such as transport arrangements
- attend routine medical appointments with the person
- provide or administer medications or treatments
- supervise the taking of medication or ensure medication/treatment compliance
- develop treatment or health care plans, or provide detailed referral information to new health care providers
- pay for medical reports or services or negotiate fees for health care interventions, where such fees apply.
For more information download the position statement titled Decisions about treatment, from the publications section below.


